What is keratoconus?
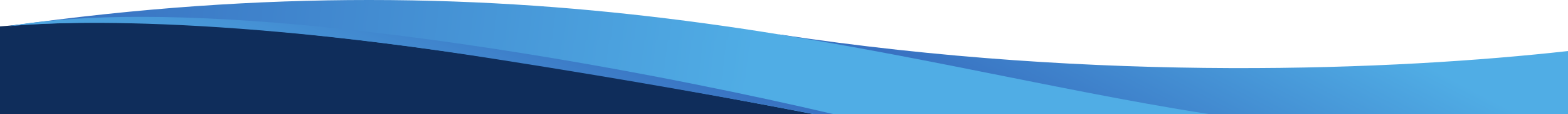
The cornea is the transparent dome-shaped window on the surface of the eye, overlying the coloured iris. Its smooth round surface is important for maintaining clear vision. In keratoconus the cornea becomes thin and distorted, eventually protruding forwards in a cone-like shape. It typically affects both eyes, but can often be quite asymmetric.
Why does keratoconus develop?
The causes of keratoconus are not very well understood. However, there is a genetic tendency, so it can sometimes run in families. There is also an association with allergies and most people with keratoconus have itchy eyes and rub their eyes to some degree. Over several years the pressure on the eye from rubbing may contribute to distortion of the cornea.
Who gets keratoconus?
Keratoconus occurs in young people, often starting in the teens, or even younger. It usually progresses slowly, and then stabilises in the twenties or thirties. It affects makes and females in all racial groups, although in New Zealand it is most common in the Maori, Pacific island and Indian populations.
What are the main symptoms of keratoconus?
Keratoconus causes blurring and distortion of vision in one or both eyes. It often gets slowly worse over time, but occasionally causes quite a sudden deterioration in vision. People with keratoconus often have associated allergic conjunctivitis, which causes itchy eyes and eye rubbing
What treatments can help with keratoconus?
There
are two main aims in treating keratoconus; improving vision and
preventing progression of the disease.
In the early stage of
keratoconus, glasses or soft contact lenses may help correct blurred
vision. As the cornea becomes more distorted only hard contact lenses
are able to improve vision. About 15% of people with keratoconus
progress to the stage where corneal transplant surgery is required.
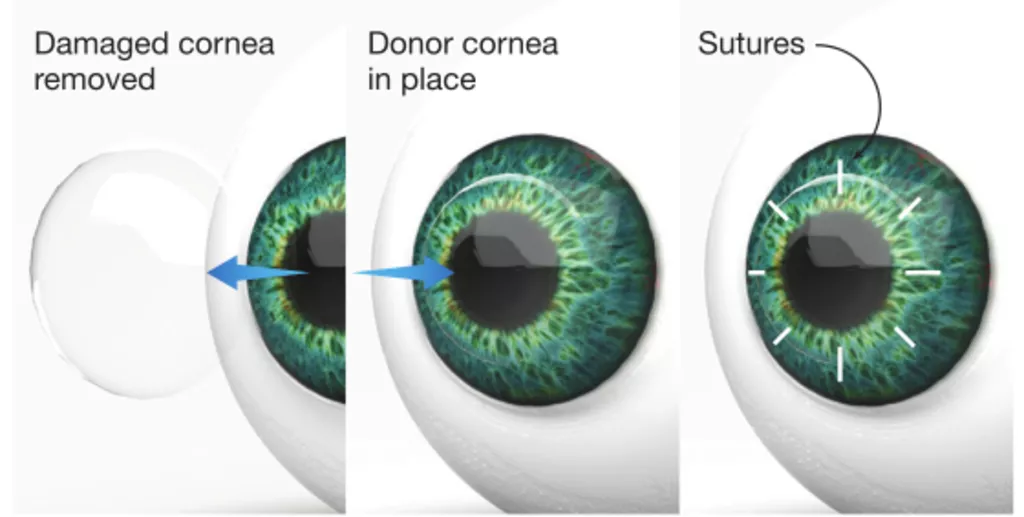
Traditionally full-thickness corneal transplant surgery has been
necessary, but in some cases of keratoconus it is now possible to
perform a partial transplant, which has advantages in long term
transplant survival.
In recent years preventing progression of
keratoconus has become a priority for people with mild or moderate
keratoconus. Treating allergic eye disease and avoiding eye rubbing
may be of some benefit.
Corneal collagen crosslinking (CXL)
CXL is a treatment designed to stabilise the disease. It uses a combination of ultraviolet light and vitaminB2 to stiffen the cornea, slowing or halting keratoconus progression. It is effective in at least 90% of cases and about 50% of people also have some improvement, with better vision and improved contact lens tolerance. CXL may reduce the need for corneal transplant surgery, by preventing keratoconus from progressing to more advanced disease.

Both CXL and Corneal Transplant operations are undertaken by Eye Doctors and we can advise which type of treatment is most suitable for you.
You can find out more information from the following websites www.nkcf.org - this is the website of the North American National Keratoconus Foundation. www.keratoconus.asn.au – this is the Keratoconus Australia website