What is Diabetic Eye Disease?
Diabetes can damage the small blood vessels in the retina at the back of the eye. If this is left untreated then permanent visual loss can occur.
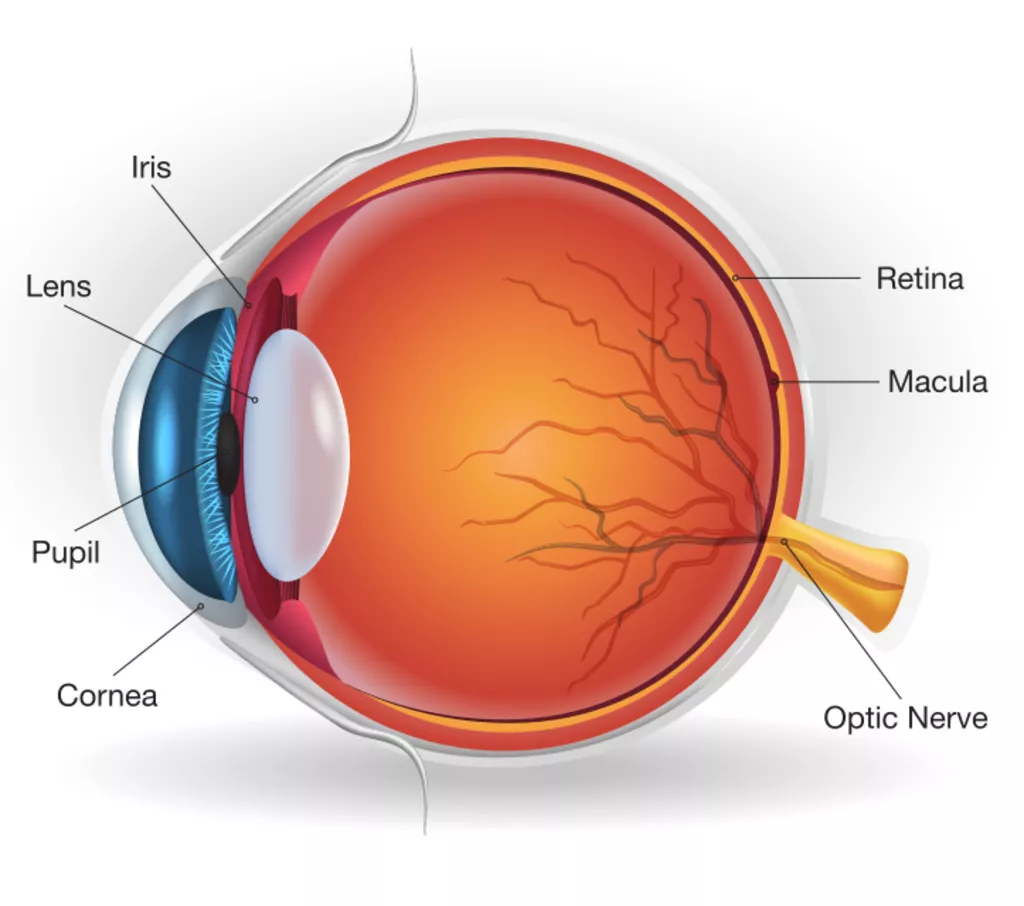
What does the retina do?
The retina is the light-sensitive nerve tissue lining the back of the eye. Like film in a video camera, the retina continually ‘take pictures’, then sends signals through the optic nerve to the brain, producing vision. The central part of the retina, which generates fine detailed vision, is known as the macula. The retina is nourished by oxygen-rich blood that is brought to it be arteries and then drained away again by veins.
What does diabetes do to the eye?
This eye has reduced vision due to leaking blood vessels at the macula (the central part of the retina). Also the peripheral retina can have abnormal blood vessel formation, bleeding and scarring. Both of these problems can lead to retinal detachment and blindness if not treated.

What are the symptoms of Diabetic Eye Disease?
Early on there are often no symptoms. Reduced vision usually occurs when severe disease has already been present for some time. Vision changes often occur gradually, but can be sudden if there is bleeding into the eye.
How is Diabetic Eye Disease detected?
Early detection is essential as the sooner the disease is treated the better the results. Your ophthalmologist will check your vision then dilate the pupils with drops. The Doctor will examine the back of your eye with a microscope. Often photos and scans are required for monitoring diabetic retinopathy. All those newly diagnosed type 2 diabetes should have a retinal check soon after diagnosis and those with type 1 diabetes should have a check within 5 years of onset. The frequency of ongoing checks then depends on the degree of retinopathy found.
Do all Diabetics get retinopathy?
Most
people with diabetes do not lose vision from diabetic
retinopathy.
Those with poor diabetic control, or who have had
diabetes for a long period of time, have higher risks of developing
the retinal complications. Other important risk factors include high
blood pressure, high cholesterol and smoking.
How is diabetic retinopathy treated?
Early diabetic retinopathy resolve with improved diabetic, blood pressure and cholesterol control. For more advanced disease treatment may be required with retinal laser and/or injections of medication into the eye, such as Avastin (Bevacizumab), Lucentis (Ranibizamab) and Eylea (Aflibercept). Rarely surgery may also be needed in sever disease.