Strabismus, commonly called squints, and amblyopia, also known as ‘lazy eye’, can both be successfully treated. The earlier they are detected the better.
SQUINT (Strabismus)
What is a squint?
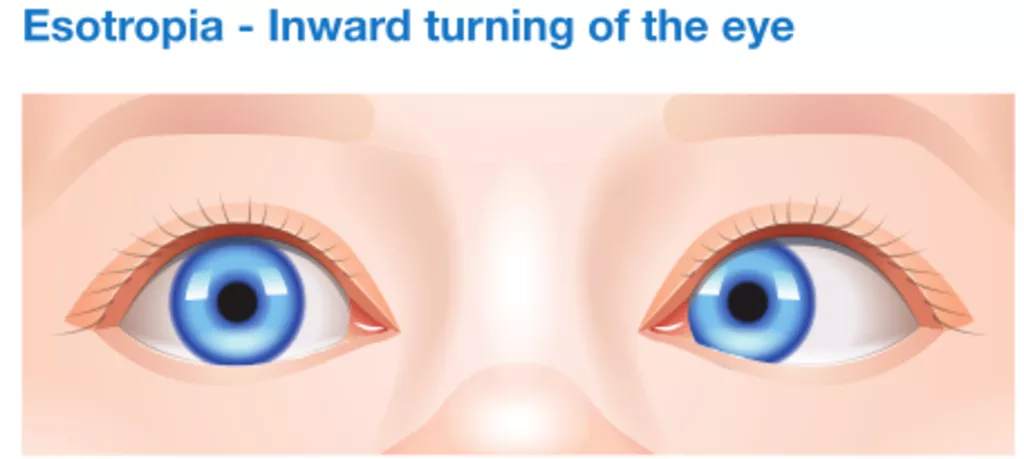
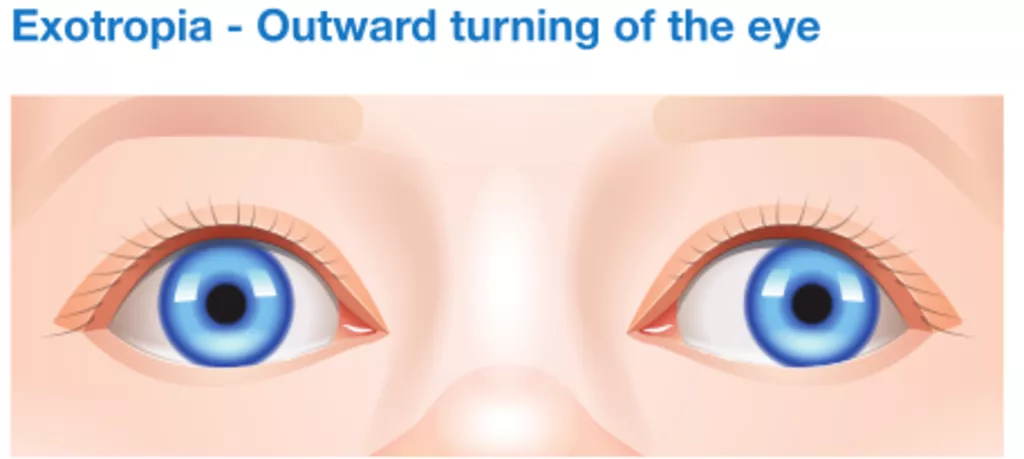
A squint is a visual defect in which the eyes are misaligned, so they point in different directions. One eye may look straight ahead, while the other eye turns inward, outward, upward and downward. The eye turn may be constant, or it may come and go. In some cases, which eye is straight (and which is misaligned) may switch or alternate.

What causes squints?
The exact cause is not fully understood. Any factors influencing the brain’s control of binocular vision, or the eye muscle functions can cause it. Occasionally squints can be associated with other conditions.
What are the signs of squints?
The main indication is that an eye is not straight. Sometime the child may turn or tilt their head to see better. Favouring one eye over the other can lead to amblyopia (lazy eye) and long term poor sight in that eye.
What is Pseudoesotropia?
The eyes of an infant may appear to be crossed, though they actually are not. This is often due to a wide, flat nose, or a fold of skin in the inner lids. Children often grow out of the pseudoesotropia but they never grow out of a true squint.
What are the most common types of squints in children?
- Infantile (or congenital) esotropia, where the eye turns inward, is the most common type of squint in infants and it usually occurs between 3-6 months of age.
- Accommodative esotropia is a common form of squint and often occurs in children two years of age, or older. The eye turns inward due to excessive focusing effort to give better vision. It can present when the child is looking at distant or near objects.
- Exotropia refers to the outward turning of the eye. This type of squint most often occurs when the child is looking at distant objects. It tends to become more noticeable when the child is tried or sick.
How are squints treated in children?
After a complete medical eye examination the child may be prescribed glasses. If glasses cannot control the squint, or are not needed then eye muscle surgery will be recommended to restore normal alignment and binocular vision (so the two eyes can work together).
How is squint surgery performed on children?
As a day stay procedure, performed under general anaesthetic. Our anaesthetists are experienced in children’s anaesthesia and surgery is performed in a fully equipped private hospital. The eye muscle causing the eye to turn inward, or outward are ‘loosened’, or ‘tightened’, as required. The eyes are not normally patched and recovery is fast so the child can resume normal activities within a few days.
When should treatment start?
Children suspected of a squint should be seen without delay by a specialist. No child is too young to be assessed and for treatment options to be discussed.
LAZY EYE (Amblyopia)
What is amblyopia?
Amblyopia is poor vision in an eye that did not develop normal sight during early childhood. It is commonly called a ‘lazy eye’.
When one eye
develops normal vision, while the other does not, the eye with poor
vision is called amblyopic. Usually only one eye is affected by
amblyopia, but it is possible for both eyes to be ‘lazy’.
This
condition is quite common, affecting approximately two or three out
of every 100 children. The development of equal vision in both eyes
is necessary for normal vision making it essential for lazy eye to be
detected and treated as early as possible in infancy or early
childhood.
What causes lazy eye?
Lazy eye is caused by any condition that affects normal use of the eyes and visual development. In many cases, the conditions associated with lazy eye may be inherited.
Lazy eye has three major causes:
- Strabismus (squint or misaligned eyes) Lazy eye occurs most commonly with misaligned or crossed eyes. The crossed eye ‘turns off’ to avoid double vision, and the child uses only the better eye. The misaligned eye then fails to develop normal vision.
- Unequal
focus and refractive errors are eye
conditions that are corrected by wearing glasses. Lazy eye occurs
when one eye is out of focus because it has more near-sight,
far-sight and astigmatism (irregular focus) than the other.
The unfocused (blurred) eye ‘turns off’ and becomes amblyopic or lazy. The eyes can look normal, but one eye has poor vision. This is the most difficult type of amblyopia to detect since the child appears to have normal vision when both eyes are open.
Lazy eye can also occur in both eyes if both eyes have very blurred vision. This can happen when there is a high amount of focus abnormality in both eyes. - Cloudiness of normally clear inner eye structures. Any factor that prevents a clear image from being focused inside the eye (like a cataract) can lead to the development on this condition in a child. This is often the most severe form of lazy eye.
How is lazy eye diagnosed?
It is not easy to recognise lazy eye. A child may not be aware of having one strong eye and one weak eye. Unless the child has a misaligned eye or other obvious abnormality, there is often no way for parents to tell that something is wrong.
Lazy eye is detected by finding a difference in vision between the two eyes or poor vision in both eyes. Special techniques are used to measure vision in young children. Your ophthalmologist often estimates vision by watching how well a baby follows objects with one eye when the other is covered, or uses picture tests in pre-schoolers. Our paediatric eye surgeon will also carefully examine the interior of the eye to see if other eye diseases may be causing decreased vision.
How is lazy eye treated?
A child must be made to use the weak eye. This is usually done by covering (patching) the strong eye for several hours per day until the vision is restored to normal or doesn’t improve any further.
Alternatively lazy eye may also be treated by blurring the vision in the good eye with special eye drops or glasses to force the child to use the lazy eye. Glasses will also be prescribed to correct errors in focusing.
If there is a cataract or other abnormality, surgery may first be required to correct the problem. An artificial intraocular lens may be implanted. After surgery, glasses or contact lenses can be used to restore focus while patching improves vision.

Early detection and early treatment
If
lazy eye is detected and treated early, most children will regain
vision. Lazy eye caused by a squint or unequal refractive errors may
be treated successfully during the first nine years of age.
If
lazy eye is not detected until after early childhood, treatment may
be not successful. Lazy eye caused by cloudiness of the eye tissue
needs to be detected and treat extremely early, within the first few
months of life, in order to be treated successfully.
NEAR-SIGHTEDNESS (Myopia)
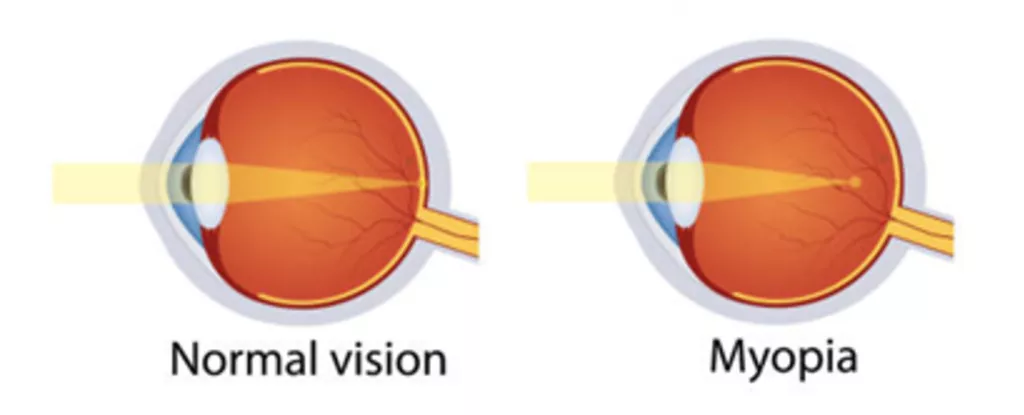
What is myopia?
Also known as near-sightedness or short-sightedness, myopia is where nearby objects are clear, while objects in the distance are blurred. This usually occurs because the eye grows too long, and light focuses in front of the retina instead of directly on it.
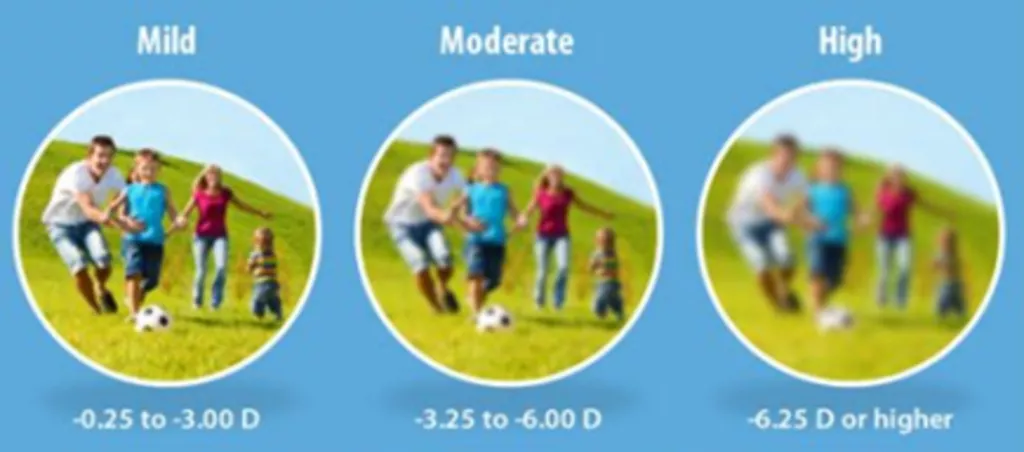
What are the symptoms of myopia?
If your child is myopic, they can have difficulty seeing things in the distance clearly, such as the whiteboard in school or people when playing sports. The severity of myopia can worsen over time as the eye continues to lengthen.
Who is affected by myopia?
The number of people in New Zealand with myopia is growing. The condition usually develops in childhood (6-13 years), when the eye is growing. It can also occur in younger children and adults.
What causes myopia?
Myopia is caused by a mix of genetic and lifestyle factors.
Children are more likely to develop myopia if their parents are myopic and if they're of East-Asian ethnicity.
Lifestyle factors include:
- Insufficient time outdoors
- Prolonged periods of looking at digital devices or doing close work
- Long durations spent in poor lighting conditions
How is myopia treated?
Myopia can be easily corrected with glasses or contact lenses. Laser surgery is an option in adults (once the myopia has stabilized).
Why is myopia control important?
Uncorrected and uncontrolled myopia can affect your child's ability to participate in school and enjoy the activities they like.
It can also lead them to having a higher glasses prescription later in life than if they were treated earlier.
Higher prescriptions lead to increased dependency on glasses, and thicker and heavier lenses that can be uncomfortable long term.
With high myopia there is also an increased risk of permanent sight-threatening conditions later in life such as:
- Retinal detachment
- Glaucoma
- Myopic retinal degeneration
- Cataract
What options are available to prevent myopia getting worse in my child?
1. Reading glasses
Correcting your child’s vision with normal glasses can slow the progression of myopia.
2. Lifestyle measures
Making environmental changes can prevent or limit the progression of your child’s myopia.
Increase time spent outdoors in natural light
- Studies have shown that spending at least 2 hours outside every day can slow myopia [1]
Limit the amount of time looking at screens and doing other close work
- Ensure the screen is positioned at a suitable distance with appropriate lighting to avoid eye strain
- Try to have regular breaks from looking at the screen. A general principle is to look every 20 minutes outside or across the room for 20 seconds.
3. Eye drops
Low doses of a drug called atropine are put into the eyes daily, in addition to wearing glasses/contact lenses. These have been shown to slow progression of myopia.[2,3] These can be prescribed by your child’s ophthalmologist and some optometrists.
4. Contact lenses
These are Orthokeratology (Ortho-K) or hard contact lenses which are worn overnight and supplied by optometrists. These alter the shape of the cornea while the child sleeps and provides temporary correction of myopia, so no glasses are required during the day. These also slow progression of myopia.[4]
5. Miyosmart glasses
These are specially designed glasses that change the focus in the peripheral vision. [5]
Each option has different advantages and disadvantages, and a multitude of factors can affect which option is most suitable for your child. As a result, discussion with your ophthalmologist can help you decide what will best meet your child’s individual needs
Is myopia management safe?
The risk of wearing contact lenses to manage myopia are similar of those of wearing traditional contact lenses. With all contact lenses there is a low risk of serious complications such as corneal infections that can cause a scar and vision loss. If your child wears contact lenses, it is important to follow strict hygiene instructions from your optometrist and have regular eye examinations.
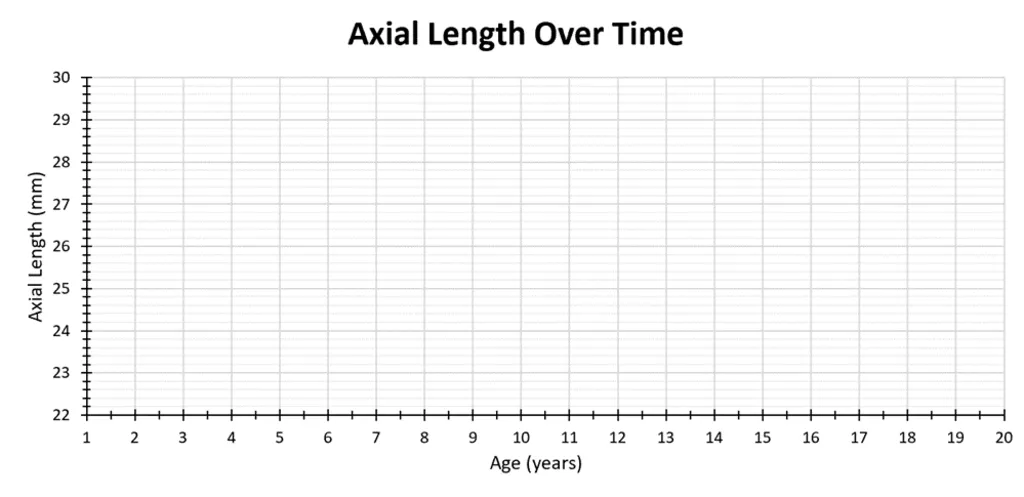
How do I know if the treatment is working?
Myopia management is unlikely to halt myopia progression entirely. Its aim is to reduce the rate of progression, compared to if there was no intervention. Regular appointments with your ophthalmologist helps to keep track of the progression of myopia. Your ophthalmologist will monitor the length of your child’s eyes, monitor their glasses prescription, and adjust treatment as necessary.
References
- Wu P, Chen C, Lin K, Sun C, Kuo C, Huang H et al. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology. 2018;125(8):1239-1250.
- Gan J, Li S, Wu S, Cao K, Ma D, He X et al. Varying Dose of Atropine in Slowing Myopia Progression in Children Over Different Follow-Up Periods by Meta-Analysis. Frontiers in Medicine. 2022;8.
- Yam J, Zhang X, Zhang Y, Wang Y, Tang S, Li F et al. Three-Year Clinical Trial of Low-Concentration Atropine for Myopia Progression (LAMP) Study: Continued Versus Washout. Ophthalmology. 2022;129(3):308-321.
- Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-Term Effect of Overnight Orthokeratology on Axial Length Elongation in Childhood Myopia: A 5-Year Follow-Up Study. Investigative Ophthalmology and Visual Science. 2012;53(7):3913.
- Lam, C., Tang, W., Lee, P., Zhang, H., Qi, H., Hasegawa, K and To, C., 2021. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow up study. British Journal of Ophthalmology, 106, pp.1110-1114.